Not Sleeping?
Undiagnosed sleep apnea can affect your ability to concentrate and leave you feeling chronically tired.
Getting Good Sleep Starts with a Home Sleep Test


Sleep Doctor
At-Home Sleep Apnea Test
Sale price
$18900
Regular price
$34900
Unit price
/
per
Single-use unit to detect both obstructive and central sleep apnea. No referral or lab visit required.
4.8
Rated 4.8 out of 5 stars
169 Reviews










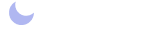
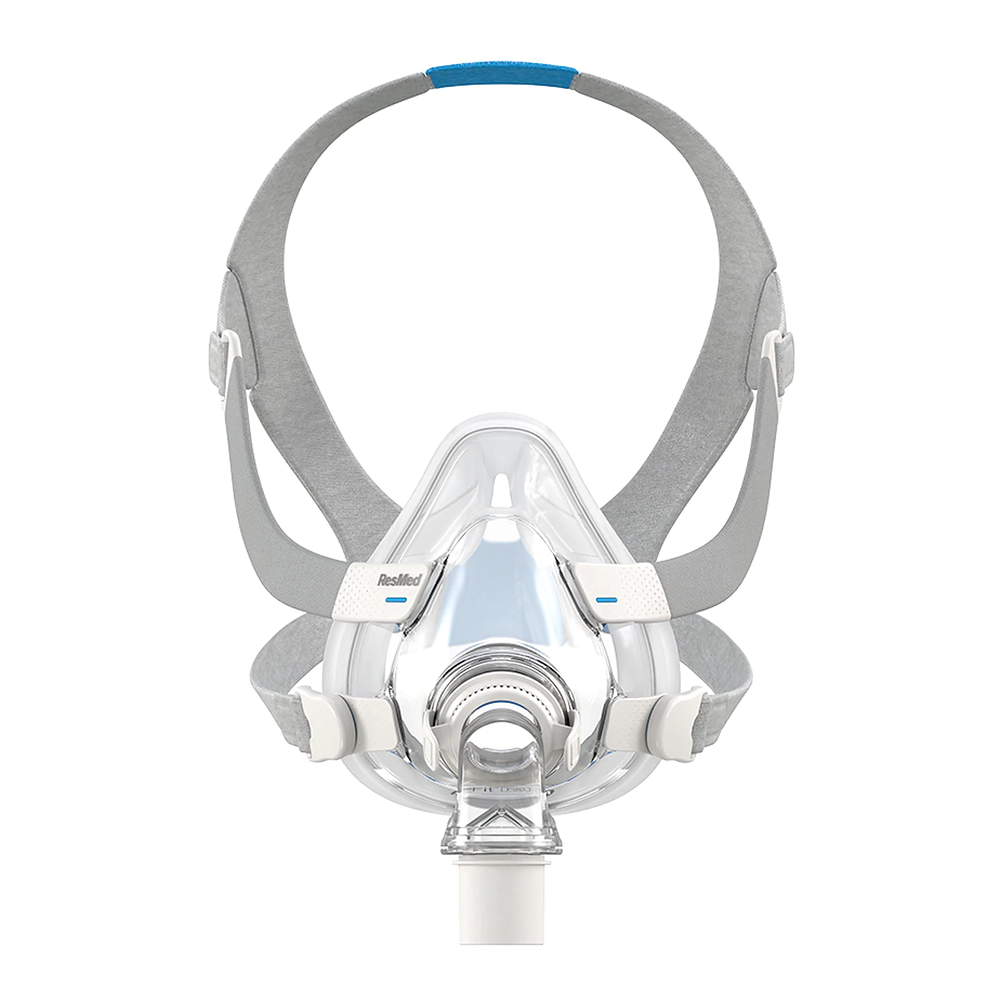
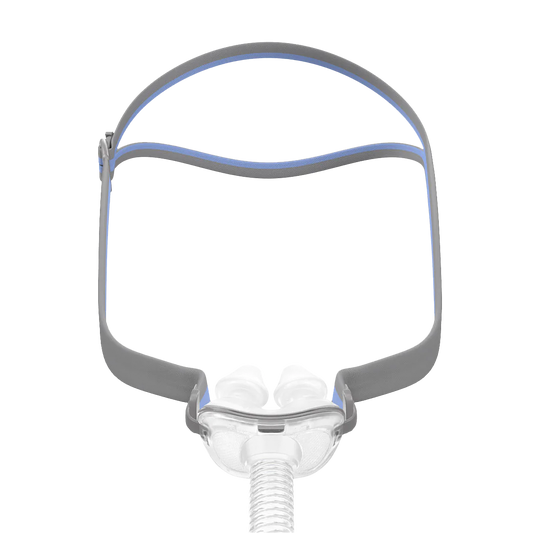
Explore CPAP Therapy and Supplies
Our Top Picks for You
-
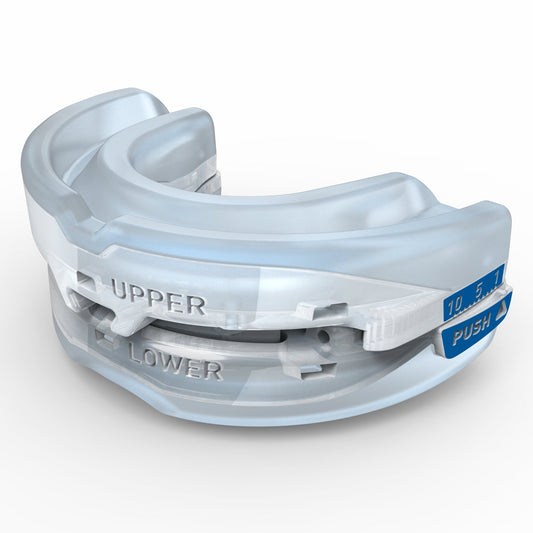
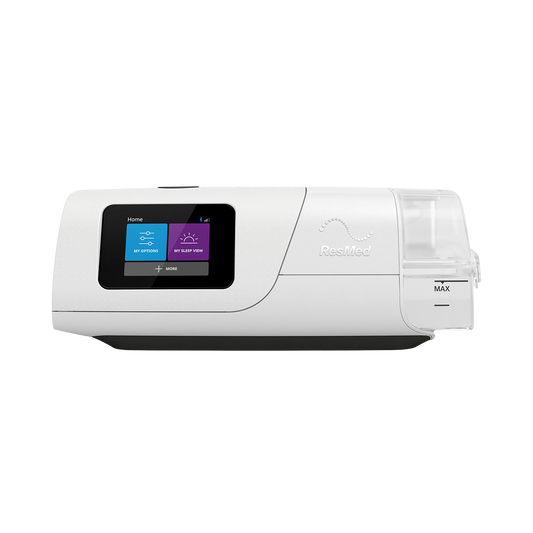
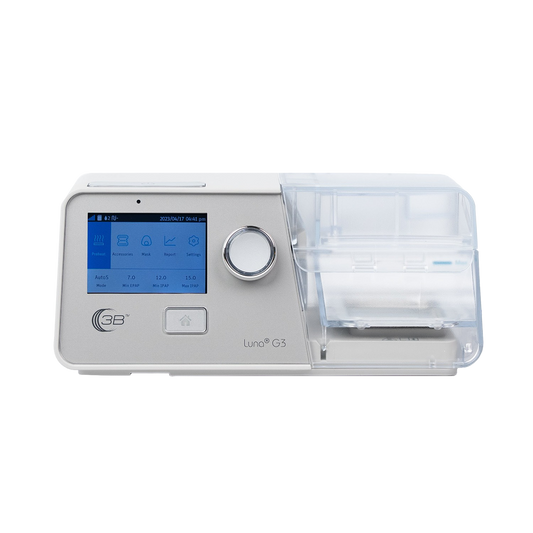
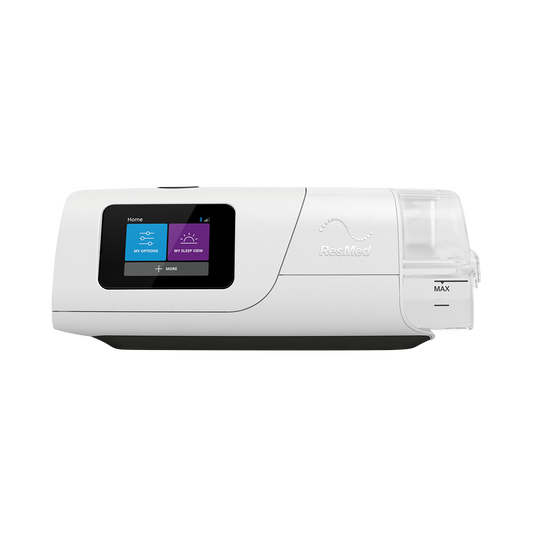
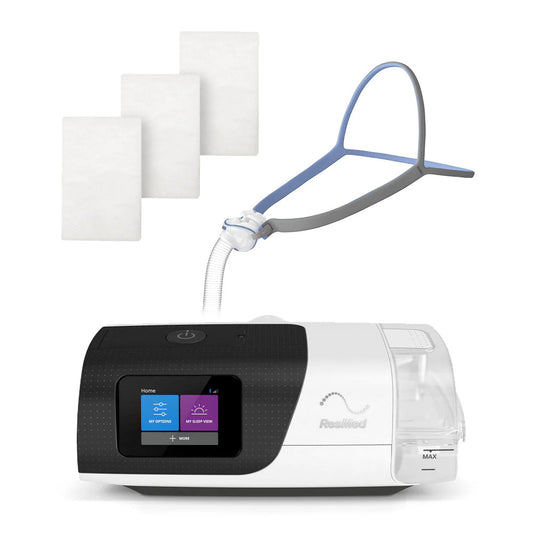
 4.9Rated 4.9 out of 5 stars14 ReviewsSale price $96000 Regular priceUnit price / per
4.9Rated 4.9 out of 5 stars14 ReviewsSale price $96000 Regular priceUnit price / per$1,16400Save -
 4.8Rated 4.8 out of 5 stars169 ReviewsSale price $18900 Regular priceUnit price / per
4.8Rated 4.8 out of 5 stars169 ReviewsSale price $18900 Regular priceUnit price / per$34900Save -
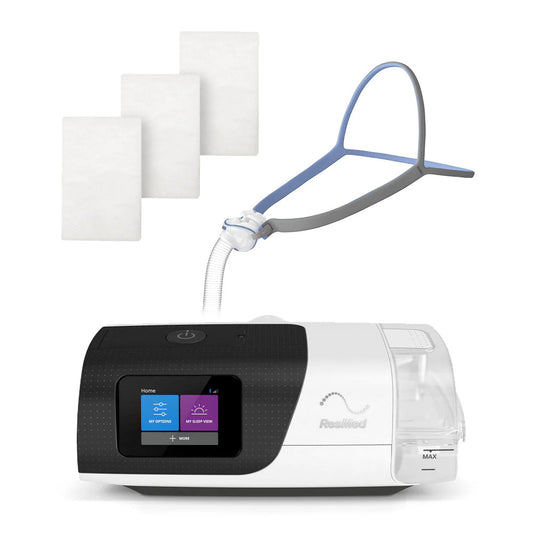
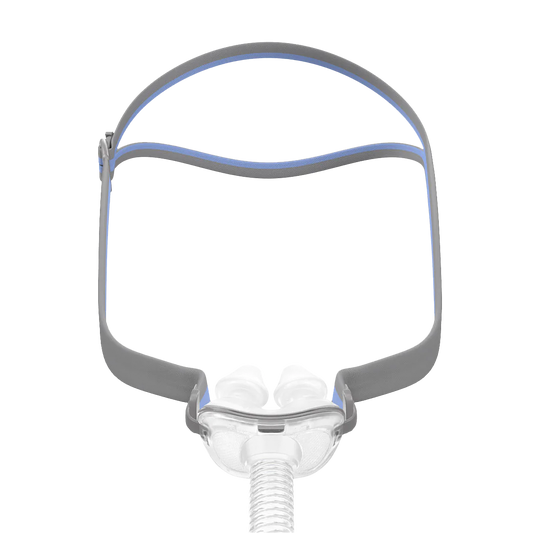
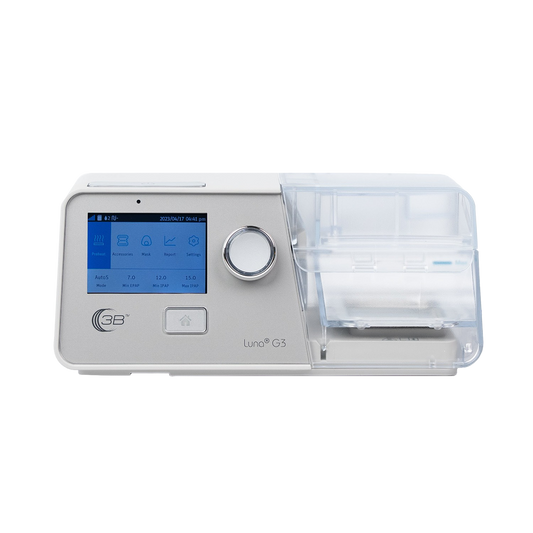
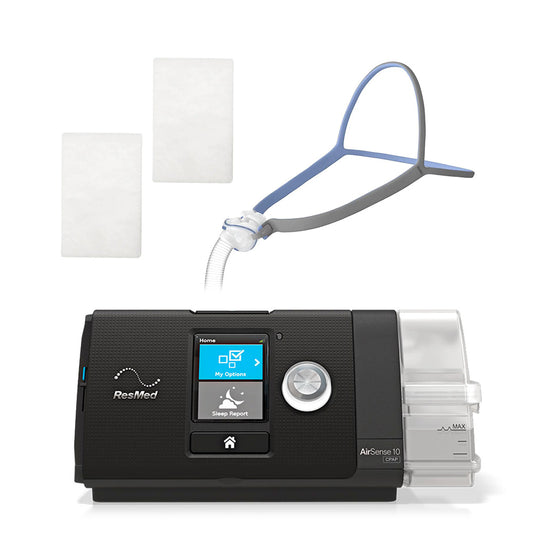
 4.8Rated 4.8 out of 5 stars12 ReviewsSale price From $91900 Regular priceUnit price / per
4.8Rated 4.8 out of 5 stars12 ReviewsSale price From $91900 Regular priceUnit price / per$1,00800Save -
 4.5Rated 4.5 out of 5 stars2 ReviewsSale price $16900 Regular priceUnit price / per
4.5Rated 4.5 out of 5 stars2 ReviewsSale price $16900 Regular priceUnit price / per$18900Save -
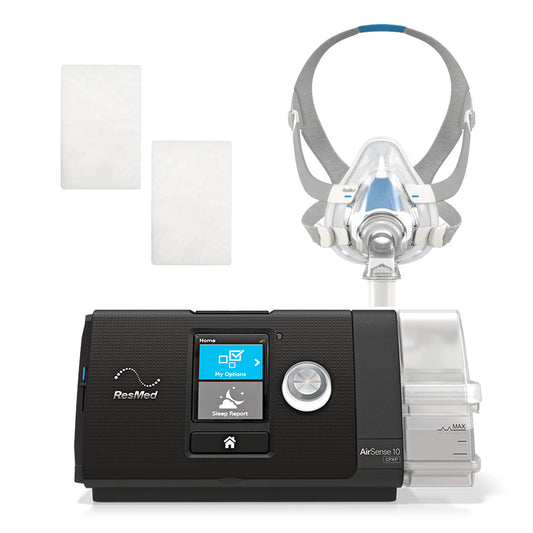
 4.6Rated 4.6 out of 5 stars28 ReviewsSale price From $1,00400 Regular priceUnit price / per
4.6Rated 4.6 out of 5 stars28 ReviewsSale price From $1,00400 Regular priceUnit price / per$1,35400Save -
 Sale price $25900 Regular priceUnit price / per
Sale price $25900 Regular priceUnit price / per$32900Save -
 5.0Rated 5.0 out of 5 stars2 ReviewsSale price $2500 Regular priceUnit price / per
5.0Rated 5.0 out of 5 stars2 ReviewsSale price $2500 Regular priceUnit price / per$3400Save -
 3.0Rated 3.0 out of 5 stars1 ReviewSale price $1100 Regular priceUnit price / per
3.0Rated 3.0 out of 5 stars1 ReviewSale price $1100 Regular priceUnit price / per -
 4.7Rated 4.7 out of 5 stars3 ReviewsSale price $79900 Regular priceUnit price / per
4.7Rated 4.7 out of 5 stars3 ReviewsSale price $79900 Regular priceUnit price / per$89900Save -
 5.0Rated 5.0 out of 5 stars8 ReviewsSale price $1,77600 Regular priceUnit price / per
5.0Rated 5.0 out of 5 stars8 ReviewsSale price $1,77600 Regular priceUnit price / per$1,99500Save -
 5.0Rated 5.0 out of 5 stars3 ReviewsSale price $4600Unit price / per
5.0Rated 5.0 out of 5 stars3 ReviewsSale price $4600Unit price / per -
 4.8Rated 4.8 out of 5 stars4 ReviewsSale price $10500 Regular priceUnit price / per
4.8Rated 4.8 out of 5 stars4 ReviewsSale price $10500 Regular priceUnit price / per -
 5.0Rated 5.0 out of 5 stars1 ReviewSale price $11500 Regular priceUnit price / per
5.0Rated 5.0 out of 5 stars1 ReviewSale price $11500 Regular priceUnit price / per -
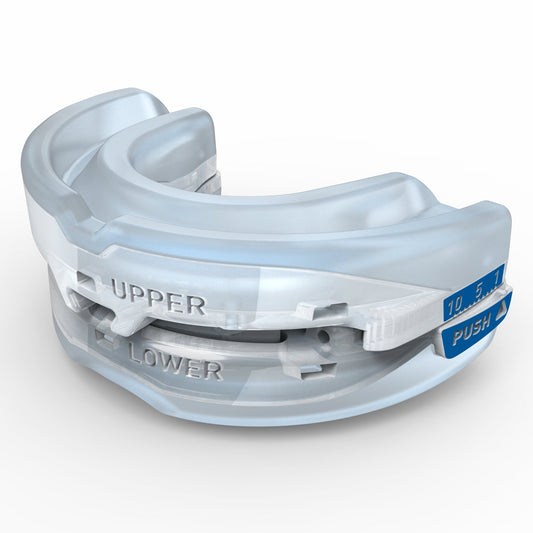 3.7Rated 3.7 out of 5 stars3 ReviewsSale price $19900 Regular priceUnit price / per
3.7Rated 3.7 out of 5 stars3 ReviewsSale price $19900 Regular priceUnit price / per$29900Save -
 Sale price $4200Unit price / per
Sale price $4200Unit price / per -
 5.0Rated 5.0 out of 5 stars2 ReviewsSale price $1,49900 Regular priceUnit price / per
5.0Rated 5.0 out of 5 stars2 ReviewsSale price $1,49900 Regular priceUnit price / per$1,89900Save -
 5.0Rated 5.0 out of 5 stars4 ReviewsSale price $84900 Regular priceUnit price / per
5.0Rated 5.0 out of 5 stars4 ReviewsSale price $84900 Regular priceUnit price / per$1,12900Save -
 Sale price $799Unit price / per
Sale price $799Unit price / per -
 Sale price Call for Price Regular priceUnit price / per
Sale price Call for Price Regular priceUnit price / per -
 Sale price $3400 Regular priceUnit price / per
Sale price $3400 Regular priceUnit price / per -
 Sale price $6200 Regular priceUnit price / per
Sale price $6200 Regular priceUnit price / per$6700Save -
 3.0Rated 3.0 out of 5 stars2 ReviewsSale price From $33900 Regular priceUnit price / per
3.0Rated 3.0 out of 5 stars2 ReviewsSale price From $33900 Regular priceUnit price / per -
 Sale price $11500 Regular priceUnit price / per
Sale price $11500 Regular priceUnit price / per$12900Save -
 Sale price $2700 Regular priceUnit price / per
Sale price $2700 Regular priceUnit price / per$3200Save -
 Sale price Call for Price Regular priceUnit price / per
Sale price Call for Price Regular priceUnit price / per -
 Sale price $2800Unit price / per
Sale price $2800Unit price / per -
 Sale price Call for PriceUnit price / per
Sale price Call for PriceUnit price / per -
 Sale price $83500 Regular priceUnit price / per
Sale price $83500 Regular priceUnit price / per$1,36500Save -
 Sale price $5400 Regular priceUnit price / per
Sale price $5400 Regular priceUnit price / per
Sleep products backed by science and rigorously tested
Recommendations you can trust
Medically reviewed products
Third-party tested and certified
Fact-checked and latest information
Most Popular CPAP Products
-
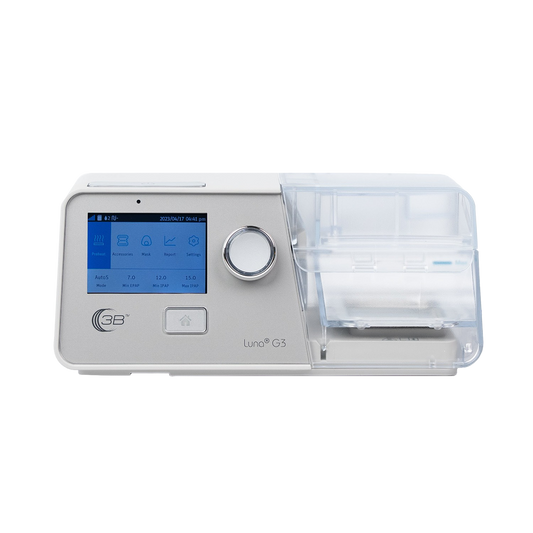
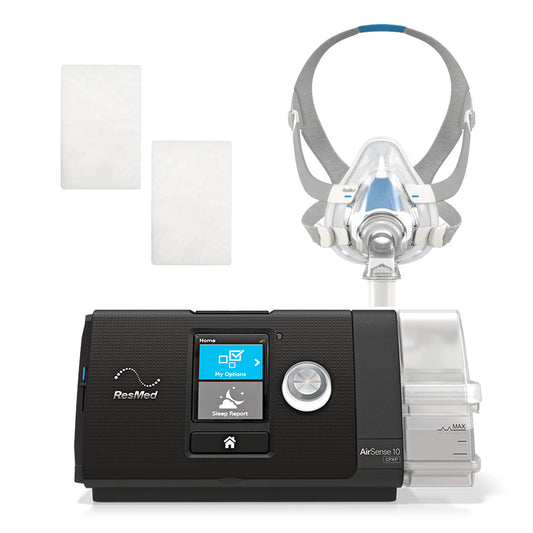
 4.9Rated 4.9 out of 5 stars14 ReviewsSale price $96000 Regular priceUnit price / per
4.9Rated 4.9 out of 5 stars14 ReviewsSale price $96000 Regular priceUnit price / per$1,16400Save -
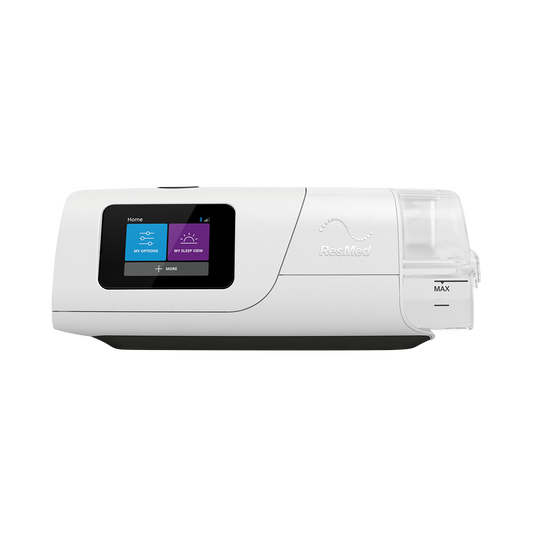
 4.6Rated 4.6 out of 5 stars28 ReviewsSale price From $1,00400 Regular priceUnit price / per
4.6Rated 4.6 out of 5 stars28 ReviewsSale price From $1,00400 Regular priceUnit price / per$1,35400Save -
 5.0Rated 5.0 out of 5 stars4 ReviewsSale price $84900 Regular priceUnit price / per
5.0Rated 5.0 out of 5 stars4 ReviewsSale price $84900 Regular priceUnit price / per$1,12900Save -
 5.0Rated 5.0 out of 5 stars8 ReviewsSale price $1,77600 Regular priceUnit price / per
5.0Rated 5.0 out of 5 stars8 ReviewsSale price $1,77600 Regular priceUnit price / per$1,99500Save -
 Sale price From $1,79600 Regular priceUnit price / per
Sale price From $1,79600 Regular priceUnit price / per -
 5.0Rated 5.0 out of 5 stars2 ReviewsSale price $1,49900 Regular priceUnit price / per
5.0Rated 5.0 out of 5 stars2 ReviewsSale price $1,49900 Regular priceUnit price / per$1,89900Save -
 Sale price Call for Price Regular priceUnit price / per
Sale price Call for Price Regular priceUnit price / per -
 Sale price Call for PriceUnit price / per
Sale price Call for PriceUnit price / per -
 Sale price Call for Price Regular priceUnit price / per
Sale price Call for Price Regular priceUnit price / per -
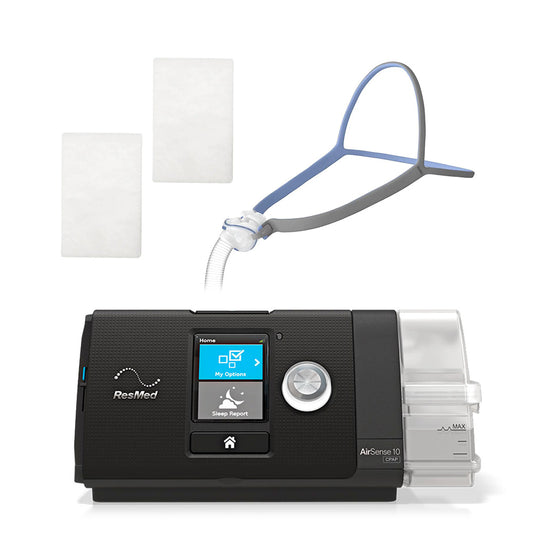
 4.8Rated 4.8 out of 5 stars12 ReviewsSale price From $91900 Regular priceUnit price / per
4.8Rated 4.8 out of 5 stars12 ReviewsSale price From $91900 Regular priceUnit price / per$1,00800Save -
 4.7Rated 4.7 out of 5 stars3 ReviewsSale price $79900 Regular priceUnit price / per
4.7Rated 4.7 out of 5 stars3 ReviewsSale price $79900 Regular priceUnit price / per$89900Save -
 5.0Rated 5.0 out of 5 stars2 ReviewsSale price $77900 Regular priceUnit price / per
5.0Rated 5.0 out of 5 stars2 ReviewsSale price $77900 Regular priceUnit price / per$99900Save -
 4.7Rated 4.7 out of 5 stars29 ReviewsSale price From $1,21000 Regular priceUnit price / per
4.7Rated 4.7 out of 5 stars29 ReviewsSale price From $1,21000 Regular priceUnit price / per$1,53500Save -
 4.7Rated 4.7 out of 5 stars32 ReviewsSale price $1,16000 Regular priceUnit price / per
4.7Rated 4.7 out of 5 stars32 ReviewsSale price $1,16000 Regular priceUnit price / per$1,47000Save -
 4.9Rated 4.9 out of 5 stars14 ReviewsSale price From $97100 Regular priceUnit price / per
4.9Rated 4.9 out of 5 stars14 ReviewsSale price From $97100 Regular priceUnit price / per$1,33000Save -
 4.9Rated 4.9 out of 5 stars18 ReviewsSale price $1,07600 Regular priceUnit price / per
4.9Rated 4.9 out of 5 stars18 ReviewsSale price $1,07600 Regular priceUnit price / per$1,28000Save -
 Sale price $83500 Regular priceUnit price / per
Sale price $83500 Regular priceUnit price / per$1,36500Save
Sleep Doctor is the only online shop I trust for the best products and recommendations. I’ve never slept better!
Janessica B.
Customer since 2017
Discover More About Sleep Apnea and CPAP
-

What is Sleep Apnea?
Read MoreSleep apnea is a common condition that affects millions of people. Find out what causes sleep apnea, who is at risk, and how it can be treated.
-

How to Find the Right CPAP Machine For You
Read MoreCPAP is the most common treatment for sleep apnea. Learn about how CPAP works, the benefits of CPAP treatment, and tips for resolving common issues.